This article is a part of your HHCN+ Membership
Since the onset of the COVID-19 emergency in early 2020, home-based care providers have had to navigate seemingly countless challenges around keeping both patients and staff safe. Providers are now gearing up to face a new and more aggressive strain of the coronavirus: the Delta variant.
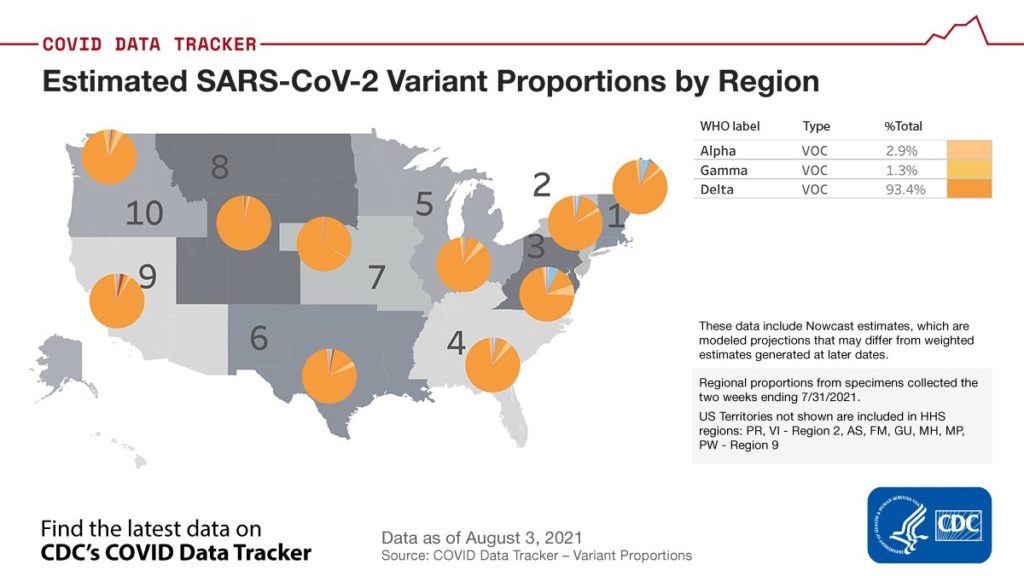
Among its major distinctions, the Delta variant is more transmissible than previous strains of coronavirus. The CDC, in fact, has classified the Delta variant as more transmissible than the common cold, influenza and the viruses that cause smallpox or Ebola.
The Delta variant has been the most dominant strain of the COVID-19 virus in India and Great Britain for some time. By the end of July, Delta cases made up more than 80% of new COVID-19 cases in the U.S., according to CDC estimates.
For home health providers, especially those in states with lower vaccination rates, all this has meant a renewed focus on infection control and staff education. Many are working tirelessly to ensure that their staff members are fully vaccinated, something that has been a challenge in the home health space, past surveys have suggested.
“We are doubling down on vaccination efforts for staff,” Brent Korte, chief home care officer at EvergreenHealth Home Care, told Home Health Care News. “We’re somewhere north of 90% for employees, including all clinicians and support staff. And we’re doubling down on this idea that we won’t rest till we get to 100%.”
Kirkland, Washington-based EvergreenHealth Home Care, a part of EvergreenHealth, is one of the largest home health and hospice providers in the Pacific Northwest. The company has a staff of roughly 600 members that manage more than 11,000 episodes of care each year.
With more than 90% of its staff vaccinated, Evergreen is in a presumably better position than its industry peers, many of which are in the midst of debating mandatory-vaccination policies.
Generally, mandatory-vaccination stances haven’t been extremely common in home health care, at least compared to other settings.
As of Tuesday, nearly one-quarter of all U.S. hospitals required staffers to get a COVID-19 vaccine. Some of the nation’s largest operators of skilled nursing facilities (SNFs) have taken that route as well, including Genesis HealthCare, which implemented a “universal” COVID-19 vaccination requirement for its employees, care partners and onsite vendors at the state of August.
“It’s a very delicate conversation — the justification and the strength behind getting vaccinated,” Korte said. “We’re at the level now where we hone in on the last maybe 8% or so of staff that can get vaccinated.”
Planning ahead
In order to address vaccine hesitancy, Korte has offered to listen to the concerns of every employee who has reservations. He recommended that other home health leaders do the same.
“No judgment whatsoever,” Korte said. “I can at least hear out and learn why they don’t want to be vaccinated, then maybe that can help me change my approach as the executive overseeing all of our work.”
In the early period of the public health emergency, Evergreen was one of the first providers in the country to treat COVID-19 patients. Being on the front line of care early has prepared Evergreen for this next phase of the pandemic, Korte explained.
“Being the first in the United States was super difficult,” he said. “The silver lining is that it forced us to prepare, it forced us to figure out personal protective equipment (PPE). It forced us to figure out proper PPE rationing. We didn’t really choose to be the tip of the spear, but it helped us not become the epicenter because we were able to take quick action. We’re using that same mentality with the Delta variant.”
In addition to Evergreen’s vaccination efforts, the company hasn’t let up on its PPE standards, still working overtime to keep its staff educated and protected. The company’s infectious disease physician, Dr. Frank Riedo, has played an integral role.
“We not so jokingly call him the Fauci of Washington State because he was the doctor that identified the first U.S. [COVID-19] patient,” Korte said. “We’re sharing his feedback. We’re super lucky as a system-based provider to have that resource. I recommend that any of the thousands of agencies out there lean on whoever that most respected, most neutral voice is.”
Another home-based care organization that is navigating the Delta variant is New York’s VNA of Albany.
VNA of Albany is a nonprofit that is affiliated with Albany Medical Center, Saratoga Hospital, Glens Falls Hospital and Columbia Memorial Hospital. As an organization, VNA of Albany offers home health and private-duty care, serving 11 counties in New York state.
Similar to Evergreen, VNA of Albany has maintained its staff PPE requirements. Keeping staff educated has also been important, as COVID-19 cases continue to rise, Holly Chaffee, VNA of Albany’s vice president and COO, told HHCN.
“It’s been educating staff that the variant is out there, encouraging them to be vigilant about hand washing, about PPE and about educating their patients,” Chaffee said. “Just because you’re vaccinated doesn’t mean this is over.”
“We didn’t really choose to be the tip of the spear, but it helped us not become the epicenter because we were able to take quick action. We’re using that same mentality with the Delta variant.”
Brent Korte, chief home care officer at EvergreenHealth Home Care
Constant communication
Among the steps it’s taking to battle the Delta variant, VNA of Albany conducts weekly team meetings with its clinicians to keep them up to date. Ensuring that VNA of Albany’s staff has been vaccinated is one of the organization’s main strategies against this latest phase of the public health emergency.
Overall, 92% of the organization’s field staff is fully vaccinated, according to Chaffee.
And while providers have mostly bounced back, many saw patient-volume decreases in the earlier part of the COVID-19 emergency. Chaffee said she doesn’t believe the Delta variant will trigger this kind of impact.
“I think it may lead to an increased volume in home health because in the skilled facilities, people were unable to visit with their family members,” she said. “Whereas, if they’re at home, they can see their family members. The isolation for patients has led to more comorbidities, loneliness and isolation, on top of other illnesses.”
Chaffee noted that a potential increase in home health volumes could result in staffing pressures on an industry that is already struggling to recruit and retain workers.
In the past week, a number of home health providers have also taken the time to address the Delta variant, with publicly traded companies doing so during their second quarter earnings calls.
Leaders from Baton Rouge, Louisiana-based Amedisys Inc. (Nasdaq: AMED), for example, said the aging-in-place giant hasn’t seen volume disruption yet, though it is seeing more staff members enter quarantine. That’s partly due to vaccine hesitancy among a relatively small portion of its workforce.
“I think the Delta variant has got people’s attention,” President and COO Chris Gerard said during a Thursday conference call. “When we do a polling of our internal staff, it’s a pretty stark line — around 20% — that are pretty opposed to taking the vaccine for various reasons.”
“Our goal is to make sure that we continue to educate and stress the importance of this,” Gerard added.
Additionally, Amedisys is watching for the potential impact the Delta variant may have on the occupancy rates at senior living facilities — a major referral source for the company. In total, senior living facilities account for about one-quarter of Amedisys referrals.
“Occupancy pressures continue to be a headwind we are fighting today, especially with the Delta variant surging and pointing to a higher probability of occupancy being significantly lower throughout the remainder of 2021,” Gerard said.
So far, the Delta variant has not impacted hiring or revenues at Frisco, Texas-based Addus HomeCare Corporation (Nasdaq: ADUS), but the company is still working to increase its staff vaccination rate, which currently sits at 60% for home health and hospice.
On the personal care side, the staff vaccination rate for Addus checks in at almost 40%.
“We’re continuing our efforts to educate our caregivers on the benefits of being vaccinated,” Bradley Bickham, executive vice president and chief operating officer of the company, said on a Q2 earnings call Tuesday. “But this is an ongoing process and certainly more challenging with a personal care workforce that is largely, part-time workers.”
“I think the Delta variant has got people’s attention.”
Chris Gerard, President and COO of Amedisys
Elective surgeries paused
Home health providers are hunkering down for another possible wave linked to the Delta variant by hammering home the importance of the vaccine, but they aren’t panicking from a business perspective.
Monday did bring a troubling sign of what the future may hold, however, as Texas Gov. Greg Abbott asked hospitals to voluntarily postpone elective surgeries due to a spike in COVID-19 cases.
“The state of Texas is taking action to combat the recent rise in COVID-19 cases and ensure that our hospitals and communities have the resources and support they need to mitigate the virus,” Abbott said.
Other states experiencing similar spikes — Arkansas, Louisiana, Florida and others — may be forced to announce similar precautions in days to come.
That could hit home health providers hard, as most saw a sharp decrease in patient volumes during the first round of elective-surgery delays.
“There’s fear in the home health community — and in the health care community, at large — that things could get tough again,” EvergreenHealth Home Care’s Korte said. “It was terrifying, what Washington state went through in March and April [2020], what New York went through a few months later and what the entire nation ended up going through. No one wants to experience that again.”
Companies featured in this article:
Addus, Amedisys, CDC, EvergreenHealth Home Care, VNA of Albany